When you’re taking antibiotics and calcium supplements, the timing could make or break your treatment. The calcium antibiotic interaction is a well-documented issue that can reduce antibiotic absorption, weaken treatment effects, and even promote resistance. This guide explores which antibiotics are affected, how the interference works, and how to time your calcium intake safely around medications.
Summary: How Calcium Affects Antibiotics
| Antibiotic Class | Affected Agents | Timing Rule (Calcium) |
|---|---|---|
| Tetracyclines | Doxycycline, Tetracycline | 2 hours before or 4-6 after |
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | 2 hours before or 6 after |
| Unaffected Agents | Amoxicillin, Azithromycin | No separation needed |
- Calcium binds to certain antibiotics in your gut, forming non-absorbable complexes.
- This includes common supplements and dairy products.
- Separation by 2–6 hours prevents reduced antibiotic efficacy.
- Alternatives like beta-lactams or non-calcium nutrients may be safer for at-risk individuals.
How Calcium Interferes with Antibiotic Absorption
Chelation: Calcium and Antibiotics Bind Together
Calcium acts as a divalent cation (Ca2+), which allows it to bind to tetracyclines and fluoroquinolones. This creates an insoluble compound in the gastrointestinal tract that your body can’t absorb. According to US Pharmacist, this is a leading cause of treatment failure for these drugs.
pH Modulation
Calcium carbonate, often used as a supplement or antacid, also raises stomach pH, making it harder for antibiotics to dissolve. This combination of chelation and delayed dissolution can significantly reduce absorption — especially for drugs like ciprofloxacin or tetracycline.
One study published in the Saudi Journal of Biological Sciences found that over 70% of hospitalized patients were co-administered calcium and antibiotics improperly, risking poor outcomes.
Antibiotics Most Affected by Calcium
Tetracyclines
- Tetracycline: Absorption can drop by up to 75%.
- Doxycycline: Less affected than tetracycline, but absorption still drops 20–30%.
- Minocycline: Interaction is less defined but still possible.
Fluoroquinolones
- Ciprofloxacin: Calcium can cut absorption by 40%.
- Levofloxacin: Reduced by 20–25%, though it’s more soluble.
- Norfloxacin: Absorption is halved, increasing treatment risk.
Aluminum or magnesium antacids make this worse, but calcium alone is still significant. For context, the mean peak plasma concentration (Cmax) of ciprofloxacin drops below the effective threshold when taken with calcium.
Learn more about how other minerals interact with antibiotics in our guide to zinc supplements and quinolone antibiotic risks.
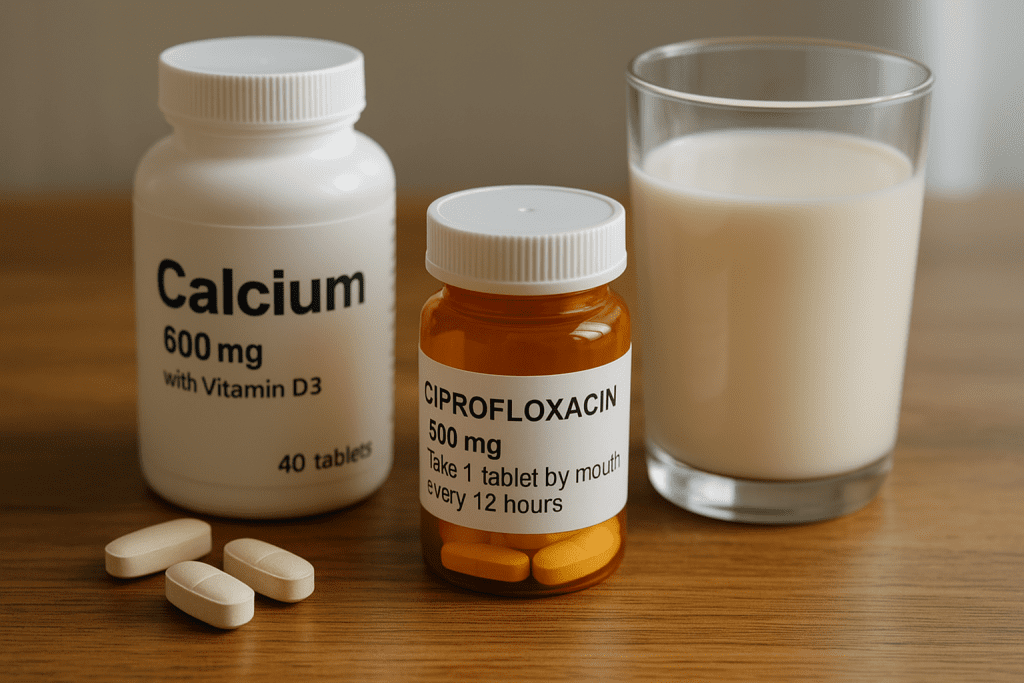
Common Sources of Calcium That Interact
It’s not just supplements. Calcium shows up in many forms:
- Dairy products: milk, cheese, yogurt
- Calcium-fortified juices
- Multivitamins
- Antacids (e.g., Tums, Rolaids)
- Mineral blends (especially those with magnesium or zinc)
Many patients unknowingly mix these with antibiotics, unaware of the absorption issue.
Clinical Impact: What Can Go Wrong
When antibiotics aren’t absorbed properly, the consequences go beyond delayed recovery.
- Treatment failure: Infections persist or worsen.
- Antibiotic resistance: Subtherapeutic levels allow bacteria to adapt.
- Worsening symptoms: Especially serious in bone or urinary infections.
For instance, E. coli can survive if ciprofloxacin levels fall below 1 µg/mL — a level easily reached if taken with calcium. This issue has led to prolonged hospitalizations and repeated courses of stronger drugs.
How to Safely Time Calcium and Antibiotics
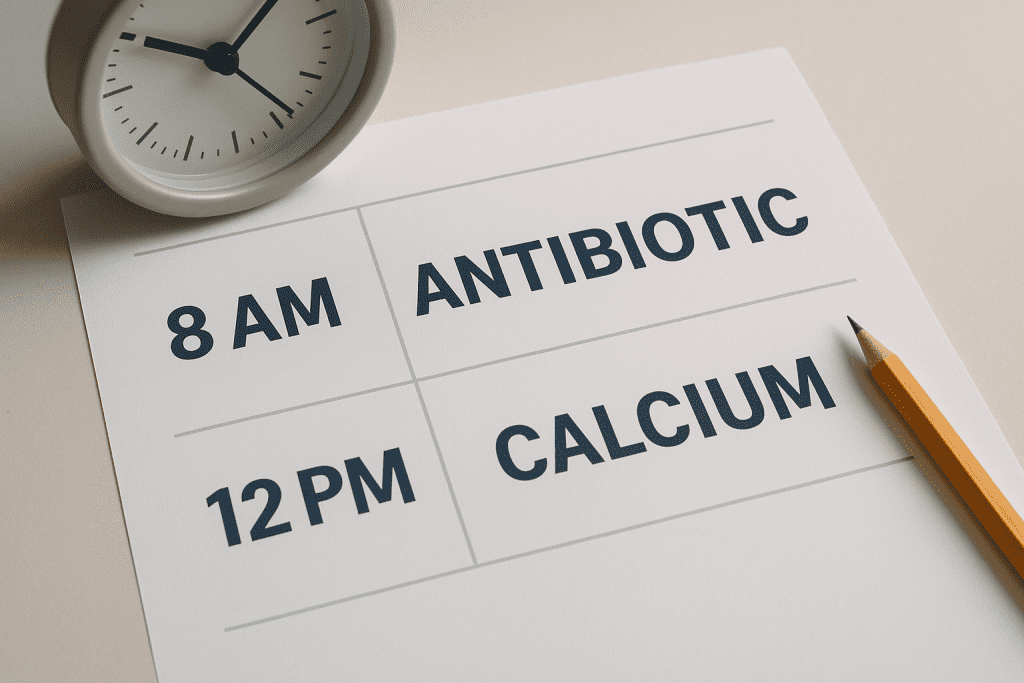
Practical Scheduling Tips
- Take antibiotics on an empty stomach with plain water
- Avoid dairy or calcium-fortified products within 2–6 hours
- If needed, schedule calcium supplements for later in the day
- Consider temporary suspension of calcium during short antibiotic courses
| Drug | Take Antibiotic | Take Calcium |
| Ciprofloxacin | 7:00 AM | 1:00 PM or later |
| Doxycycline | 8:00 AM | 12:00 PM |
Mount Sinai recommends separating doses by at least 4 hours for fluoroquinolones and 2 hours for doxycycline.
Alternatives for Patients at Higher Risk
For those who can’t modify their supplement schedule:
- Switch antibiotics: Azithromycin or amoxicillin are not calcium-sensitive.
- Try calcium-free multivitamins during the course
- Use dietary alternatives like leafy greens or topical calcium if needed
This is especially important for older adults, osteoporosis patients, and those with kidney issues where proper drug levels are critical.
Conclusion: Timing Calcium Right for Effective Antibiotic Therapy
The calcium antibiotic interaction is easy to overlook — but the consequences can be serious. Whether from a supplement or your morning yogurt, calcium can block antibiotic absorption and compromise your recovery. By separating these doses appropriately, you can ensure that both your bone health and infection treatment stay on track.
For more information, explore our related guide on zinc supplements and quinolone antibiotic risks.


Pingback: Zinc Antibiotic Nausea: How to Ease GI Distress [Expert Guide] | Useful Vitamins
Pingback: Check OTC Drug Supplement Interactions [Expert Guide] | Useful Vitamins