Many people worry about headaches after taking vitamin B with antidepressants and wonder if there’s a real connection. This concern often stems from overlapping effects on the central nervous system or fears about heightened side effects. Yet, the scientific consensus suggests that B vitamins—especially vitamins B6 and B12—are generally safe and may even complement antidepressant therapy.
In this article, the focus is on whether vitamin B supplementation can actually trigger headaches, how it might influence antidepressant efficacy, and what research-based strategies can help you safely combine them. By the end, you’ll know the key facts, potential benefits, and best practices to avoid unnecessary discomfort.
Quick Summary: Are Headaches After Taking Vitamin B With Antidepressants Common?
- Minimal evidence supports the idea that vitamin B triggers headaches when combined with SSRIs or other antidepressants.
- Certain studies indicate that B vitamins might enhance antidepressant effects and help with migraines.
- Proper dosage matters: Too much or too little vitamin B can sometimes produce headaches or other side effects.
- Individual factors—like existing vitamin deficiencies or other health conditions—play a significant role.
- Consult a healthcare professional if you experience persistent headaches, as the cause might stem from multiple factors (including medication changes, lifestyle shifts, or underlying health issues).
Overall, “headaches after taking vitamin B with antidepressants” is a relatively rare phenomenon, and most research points to a neutral or beneficial impact on mood and headache frequency.
Why Do Some People Experience Headaches After Taking Vitamin B With Antidepressants?

Understanding the Overlap of Nutritional and Pharmacological Effects
One possible explanation for experiencing headaches after taking vitamin B with antidepressants relates to how both components might interact within the nervous system. Antidepressants, especially selective serotonin reuptake inhibitors (SSRIs), adjust the levels of neurotransmitters—like serotonin—responsible for mood regulation. Meanwhile, B vitamins (including vitamin B6 and vitamin B12) are key players in metabolic pathways that also influence serotonin and other neurotransmitters.
A few individuals become alarmed if they notice a short-term headache while introducing a new vitamin supplement. However, this symptom often emerges from the body’s initial adjustment to a fresh nutrient balance. According to a drug interaction report by Drugs.com, SSRIs such as sertraline typically show no direct interaction with vitamin B12 or vitamin B6. In other words, they don’t commonly cause pharmacological conflicts that would provoke headaches.
Possible Causes of Headaches
- Dosage-Related Factors: Large doses of certain B vitamins, including B6, can in rare cases cause neuropathic symptoms or headaches when taken excessively.
- Individual Sensitivity: Some people are more sensitive to any change in routine—dietary, supplemental, or medicinal.
- Underlying Deficiencies: Low folic acid or vitamin B12 levels can contribute to neurological symptoms, including migraines, so any shift toward restoring normal levels could temporarily trigger bodily reactions.
- Other Medications: If you’re taking multiple prescriptions, be aware of synergy or interference. For example, vitamin B6 levodopa Parkinson’s interference is a recognized phenomenon, indicating that even essential vitamins can affect drug metabolism under specific conditions.
Migraines, Vitamin B, and Clinical Research
A handful of randomized controlled or placebo-controlled trials have explored the link between B vitamins and migraine headaches. In one study reviewing vitamin B supplementation, participants reported fewer migraines and a drop in severity when vitamins like B6, B12, and folate were added to their regimen. Another team at a university of medical sciences found that homocysteine levels—related to folate and B12 status—played a role in migraine intensity. By rebalancing these vitamins, people with a risk of depression and frequent headaches often noticed improvements.
To learn more about how B vitamins could potentially influence brain fog and related symptoms, consider checking out brain fog from B vitamins and migraine medication. There, we dive deeper into how nutritional components tie into cognitive clarity.
Potential Benefits and Interactions of Vitamin B and Antidepressant Use
Strengthening Mood and Alleviating Side Effects
A question often raised is whether vitamin B supplementation—particularly vitamin B6 or vitamin B12—provides real-world benefits for those on antidepressants. Evidence suggests that these nutrients can boost the response to antidepressant medications when someone has a confirmed deficiency or low vitamin status.
One large randomized controlled study reported in a PubMed-indexed publication discovered that b vitamin supplementation did not enhance immediate antidepressant results at 12 weeks. However, it did sustain and extend antidepressant benefits over the course of a year. This finding implies that while you may not feel changes overnight, consistently adequate B vitamin levels might support longer-term mental health improvements.
Addressing Headaches and Migraines
Rather than causing headaches, b complex supplements could actually help in managing them. In research focused on migraine headaches, nutrients like vitamin B12 and folic acid appear to lower homocysteine levels, which might reduce headache frequency. Studies also suggest that adequate vitamin B6 can assist with the synthesis of neurotransmitters involved in pain regulation.
It’s worth noting that people with migraines sometimes take antidepressants for off-label headache management. The Mayo Clinic acknowledges that certain antidepressants can help in migraine prophylaxis, although the mechanism likely differs from their action on mood. Given that the pathways of both vitamins and antidepressants converge on neurotransmitter activity, it’s plausible that synergy (rather than conflict) is often the outcome.
Other Complementary Approaches
Combining vitamin B with antidepressants is just one piece of the puzzle. Lifestyle factors such as hydration, sleep quality, and stress management all influence headache patterns. Some individuals explore alternative supplements—like 5-HTP—to boost serotonin, but that raises concerns about serotonin syndrome. If you’re curious about this, see antidepressants and 5-HTP serotonin syndrome risk, which covers how mixing certain supplements with prescription meds can lead to unwanted side effects.
When it comes to broader supplementation and drug interactions, even nutrients with beneficial reputations can complicate medication absorption. For example, vitamin C and Adderall absorption interaction might lead to suboptimal dosing outcomes. So, staying informed is key to maximizing benefits and minimizing complications.
Pro Tips for Safe Use of Vitamin B Supplements With Antidepressants
1. Get a Baseline Check
Start by checking your vitamin B12, folic acid, and vitamin B6 levels through blood tests. This step offers clarity on whether you genuinely need supplementation, and it helps you track improvements. The Office of Dietary Supplements provides recommended daily allowances, ensuring you stay in a safe and effective range.
2. Introduce Supplements Gradually
If you’re worried about headaches after taking vitamin B with antidepressants, ease into a new supplement routine by starting with a lower dose. Gradual adjustments give your system time to adapt and can reveal any sensitivity without overwhelming your daily routine.
3. Pay Attention to Timing
Some prefer taking B vitamins in the morning to prevent overstimulation at night. Others might combine them with meals to offset possible stomach discomfort. That said, each individual responds uniquely, so a bit of trial and error (guided by your healthcare provider) helps you find an optimal schedule.
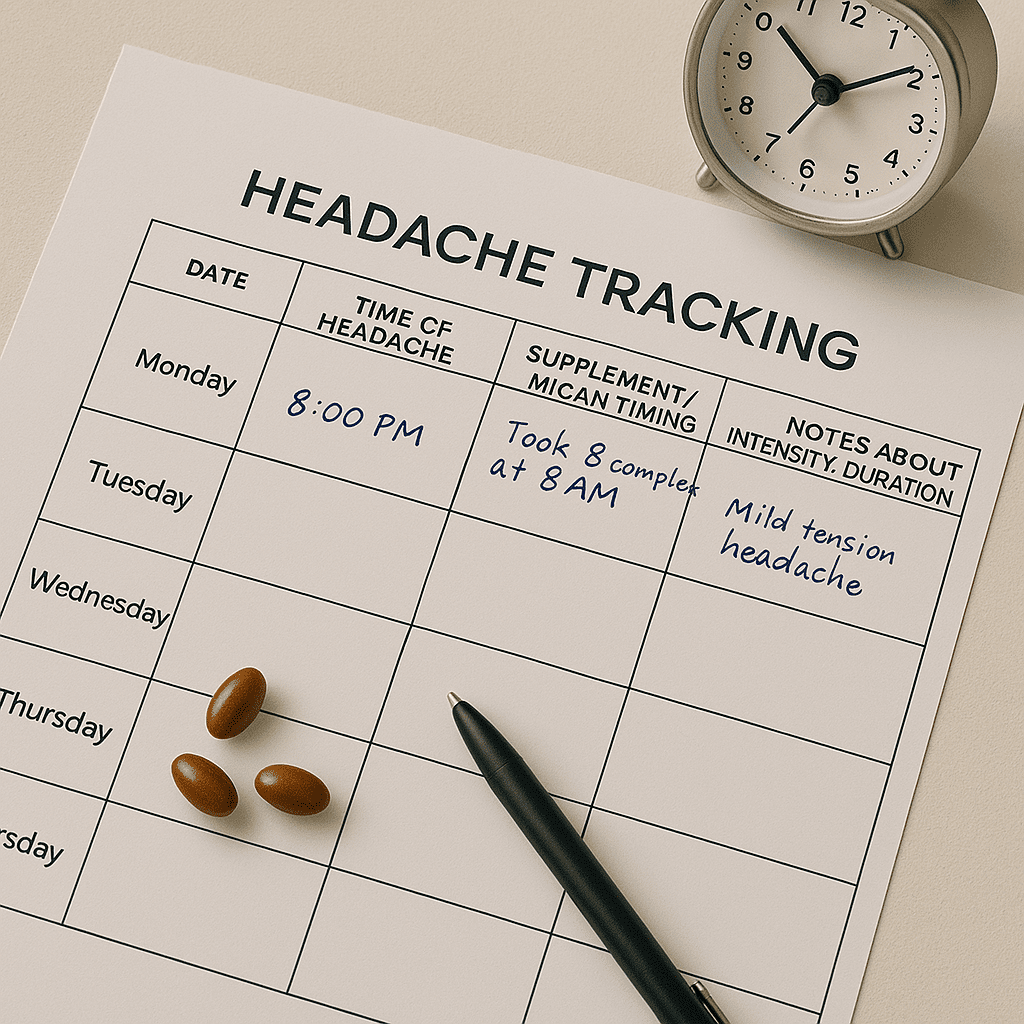
4. Monitor Headache Patterns
Keep a simple journal or use a health-tracking app to note when headaches occur relative to supplement intake and medication timing. If you spot a consistent pattern, bring those details to your next medical appointment. This record can be invaluable in pinpointing whether the headache is linked to B vitamins, the antidepressant, or unrelated factors like stress or dehydration.
Sample Headache-Tracking Table
| Day | Time of Headache | Supplement/Med Timing | Notes (Intensity, Duration) |
|---|---|---|---|
| 1 | 2 PM | Took B complex at 8 AM | Mild tension headache |
| 2 | None | Medication only | No issues, normal day |
Regular tracking builds a clearer picture, helping you and your healthcare team make data-driven decisions.
5. Ask About Possible Drug Interactions
Though SSRIs rarely conflict with B vitamins, other classes like monoamine oxidase inhibitors (MAOIs) can lower vitamin B6 levels. And certain combos, such as insomnia from St. John’s Wort and SSRIs, might amplify side effects. This is why open dialogue with a pharmacist or physician is so crucial.
Conclusion
Headaches after taking vitamin B with antidepressants remain relatively rare, with most evidence pointing toward a neutral or beneficial effect of B vitamin supplementation. For those experiencing migraines or tension-type headaches, ensuring adequate levels of B6, B12, and folate may actually help reduce frequency or intensity. Proper dosing, consistent monitoring, and professional guidance are essential to ensure any supplement integrates smoothly with prescribed medications.
Curious about other ways vitamins might impact everyday health? Feel free to explore more topics on UsefulVitamins.com, where we delve into evidence-based strategies for optimizing wellness through targeted nutrition. By staying informed and proactive, you can safely reap the benefits of both antidepressants and vitamin B—often without the dreaded headache.
Disclaimer: This content is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider before making changes to your supplement or medication routine.

