
Why You Should Be Concerned About Potassium and ACE Inhibitors
ACE inhibitors are cornerstone medications for conditions like high blood pressure, heart failure, and chronic kidney disease. But their interaction with potassium—especially through supplements or high-potassium foods—can be dangerous. This guide breaks down the key facts about the potassium ACE inhibitor interaction, outlines signs of hyperkalemia (high blood potassium), explains when potassium meds with lisinopril are risky, and highlights safe practices for monitoring and supplementation.
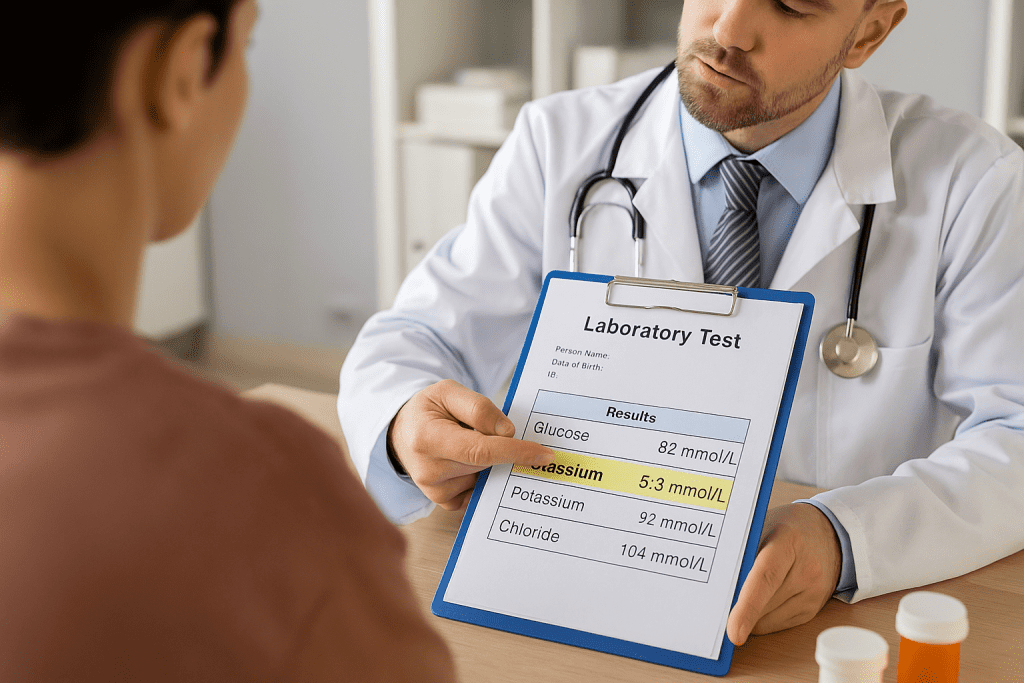
Quick Summary: Are Potassium Supplements Safe with ACE Inhibitors?
| Key Consideration | Safe or Risky? |
|---|---|
| Baseline potassium < 4.5 mmol/L | Typically safe, with monitoring |
| Potassium 5.0–5.5 mmol/L on ACE inhibitor | Monitor closely; avoid supplements |
| Potassium > 5.5 mmol/L | High risk—supplementation unsafe |
| Coexisting kidney disease or diabetes | Elevated hyperkalemia risk |
| Using potassium-sparing diuretics | Increases danger significantly |
| Salt substitutes or muscle supplements | Often risky when on ACE inhibitors |
Patients on ACE inhibitors like lisinopril should avoid potassium supplementation unless advised by a doctor. Monitoring through regular blood tests is essential.
How ACE Inhibitors Affect Potassium Regulation
ACE inhibitors work by blocking the renin-angiotensin-aldosterone system (RAAS), which in turn reduces blood pressure and protects the heart and kidneys. However, this process also decreases aldosterone—a hormone that helps excrete potassium via the kidneys.
When aldosterone drops, the body retains more potassium. This is usually safe in healthy individuals, but in people with underlying kidney disease or other risk factors, potassium can quickly accumulate to dangerous levels.
Why High Potassium Is Dangerous
Hyperkalemia can cause:
- Muscle weakness
- Nausea
- Irregular heart rhythms
- In severe cases, cardiac arrest
Symptoms often appear only after levels become critically high, making routine monitoring essential for anyone on an ACE inhibitor.
According to the American Heart Association, even mild elevations in potassium (>5.0 mmol/L) can increase cardiovascular risk.
Monitoring Guidelines: What Specialists Recommend
How Often Should Potassium Be Checked?
Nephrologists and cardiologists recommend a structured monitoring plan:
- Before starting therapy to assess baseline potassium and kidney function
- Within 1 week of starting or changing dose
- Every 4 months during ongoing treatment
KDIGO (Kidney Disease: Improving Global Outcomes) guidelines emphasize checking potassium and GFR within one week of ACE inhibitor initiation. The KDOQI guidelines offer a risk-stratified approach:
- High-risk patients (e.g., eGFR <60 or potassium >4.5 mmol/L): test in 1–4 weeks
- Lower-risk patients: test within 4–12 weeks
Cardiologists, including those from the American College of Cardiology, also recommend monitoring serum electrolytes and creatinine within a week of initiation.
Risk Factors That Raise Hyperkalemia Risk with ACE Inhibitors
Patient-Specific Risk Factors
- Reduced Kidney Function: With impaired kidney excretion, potassium levels can spike rapidly
- Diabetes and Heart Failure: Both increase susceptibility to hyperkalemia
- Baseline Potassium >4.5 mmol/L: Each 0.1 mmol/L increase raises hyperkalemia risk by nearly 20%, as shown in JAHA research
Medication-Related Risk Factors
- Potassium-Sparing Diuretics: Significantly elevate potassium risk
- Dual RAAS Blockade (ACEI + ARB): Now discouraged due to increased adverse events
- NSAIDs or Heparin: May compound potassium retention
If you’re also using diuretics, learn more in Muscle cramps from diuretics and potassium supplements.
When Potassium Supplements Become Dangerous
Potassium supplements—whether in tablet, powder, or salt-substitute form—can quickly push potassium into a dangerous range for ACE inhibitor users.
High-Risk Scenarios
- Baseline potassium >5.0 mmol/L: According to NICE guidelines, avoid initiating ACE inhibitors
- Chronic Kidney Disease (CKD): Impaired excretion amplifies supplement risk
- Stacked Risks: Combining ACE inhibitors with diuretics, NSAIDs, or a high-potassium diet
A report from WebMD cautions against using potassium salt substitutes or muscle-building supplements alongside ACE inhibitors.
Supplements, Salt Substitutes, and Diet
Many over-the-counter products labeled “heart-healthy” or “low sodium” contain potassium chloride. These can be extremely risky when combined with medications like lisinopril.
Can I take magnesium with blood pressure medication? explores similar interactions with common supplements and is worth reviewing if you’re managing multiple conditions.
Managing Elevated Potassium While on ACE Inhibitors
What happens if potassium rises too high?

Stepwise Response
- Identify the source: Evaluate recent diet changes, medications, or supplements
- Dose adjustment: Reduce ACE inhibitor dose by 50% and recheck labs in 1–2 weeks
- Further action: If still elevated, consider medication switch or stopping the ACEI
Dietary counseling and adding a thiazide or loop diuretic can help offset potassium retention. As per Cleveland Clinic Journal of Medicine, potassium should be re-evaluated within 10–14 days after any intervention.
Conclusion: Practical Takeaways for ACE Inhibitor Users
- Always check baseline potassium and kidney function before starting ACE inhibitors
- Avoid potassium supplements or salt substitutes unless prescribed
- Regular monitoring is essential, especially in patients with kidney disease or diabetes
- Work with your doctor to adjust medications if potassium starts creeping up
For related concerns, explore Muscle cramps from diuretics and potassium supplements to understand the broader picture of electrolyte balance and supplement safety.


Pingback: Water Intake Tracker Electrolyte Warning [Expert Guide] | Useful Vitamins