Antibiotics can disrupt your gut microbiome—but taking probiotics at the right time can help maintain balance and prevent digestive issues. This guide explores the best timing for probiotics with antibiotics, which strains are most effective, and how long to continue them for optimal gut flora management.
Quick Summary: Best Timing for Probiotics with Antibiotics
| Factor | Recommendation |
|---|---|
| Start Timing | Begin probiotics the same day as antibiotics |
| Daily Spacing | Take probiotics 2–4 hours after your antibiotic dose |
| Post-Antibiotic Duration | Continue probiotics for 1–2 weeks after finishing antibiotics |
| Top Strains | Saccharomyces boulardii, Lactobacillus rhamnosus GG, Bifidobacterium lactis |
| Best Doses | 10–20 billion CFUs daily, especially in higher-risk individuals |
Taking probiotics during antibiotic treatment can help reduce risks like antibiotic-associated diarrhea (AAD) and support long-term gut health.
Why Antibiotics Disrupt Gut Flora
Antibiotics are designed to kill harmful bacteria—but they’re often indiscriminate, wiping out beneficial gut microbes as well. This disruption can lead to side effects like bloating, diarrhea, and even overgrowth of harmful bacteria like Clostridioides difficile.
The gut microbiome plays a central role in digestion, immunity, and even mood regulation. Studies published in journals like BMJ Open and Frontiers in Medicine have shown that gut microbial diversity can remain suppressed for weeks to months after antibiotic use.
This is where probiotics come in. When taken correctly, they can help replenish beneficial bacteria, restore balance, and reduce complications.
Optimal Timing for Taking Probiotics with Antibiotics

Start on the Same Day
Experts recommend beginning probiotics the same day you start your antibiotics. This approach provides early support to your gut ecosystem before damage escalates. According to Symprove’s clinical resources and guidelines by the International Scientific Association for Probiotics and Prebiotics, starting immediately helps preserve microbial diversity.
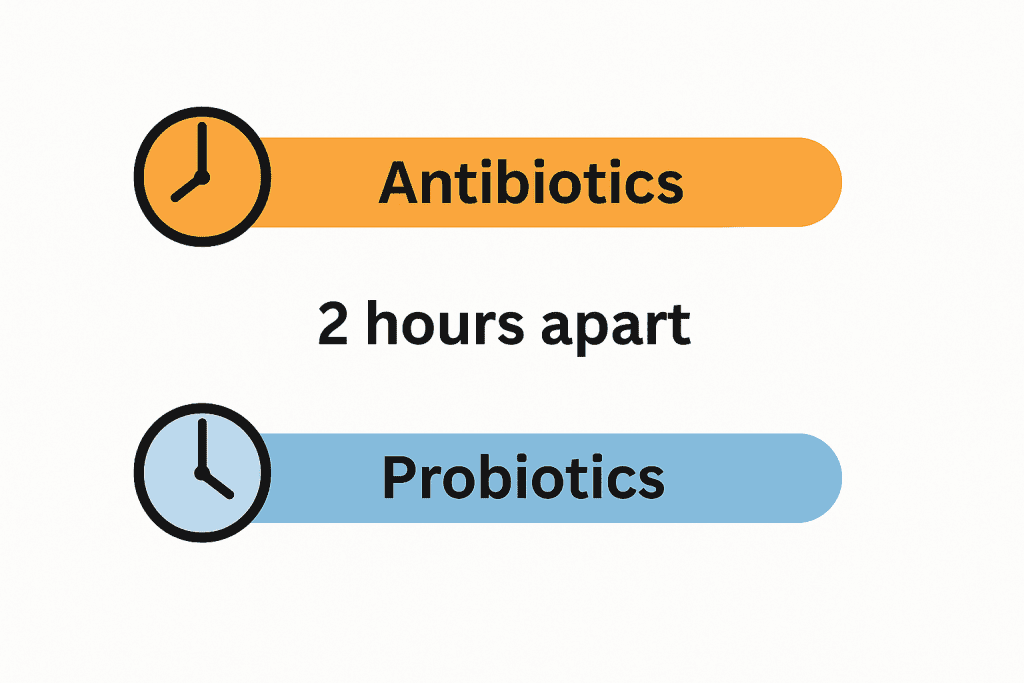
Space Your Doses by 2–4 Hours
To maximize effectiveness, avoid taking your probiotic and antibiotic doses at the same time. Antibiotics can kill the live organisms in probiotics if taken together.
Best practice:
Take your probiotic 2–4 hours after your antibiotic dose. For example, if your antibiotic is at 8 a.m. and 8 p.m., take your probiotic at 11 a.m. and 11 p.m.
This spacing minimizes interference and allows the probiotic strains a better chance to survive the journey through your digestive tract. Some studies, such as those reviewed by BuzzRx and the Beds Formulary, suggest that spacing doses can significantly improve probiotic efficacy.
Continue for 1–2 Weeks After
Even after your antibiotic course ends, your gut isn’t fully recovered. Probiotic supplementation for at least one to two weeks after antibiotics helps re-establish a healthy microbial community.
In fact, research published in BMJ Open notes that microbiome disturbances may last up to two years post-antibiotics, though symptoms often subside sooner.
The Most Effective Probiotic Strains
Not all probiotics are created equal. Specific strains have been studied for their ability to reduce antibiotic-associated symptoms and restore microbiome health.
1. Saccharomyces boulardii (S. boulardii I-745)
This beneficial yeast is naturally resistant to antibiotics, making it ideal for concurrent use.
- Multiple meta-analyses in PubMed and Medical News Today confirm its effectiveness in reducing AAD, especially in children and hospitalized adults.
- The I-745 strain shows particular promise for preventing Clostridium difficile-associated diarrhea, a serious post-antibiotic complication.
2. Lactobacillus rhamnosus GG (LGG)
One of the most clinically studied probiotic strains:
- Proven to reduce antibiotic-associated diarrhea and gastrointestinal complaints in children and adults, as documented in the Journal of Pediatrics and PLoS ONE.
- Helps maintain microbial balance during penicillin and macrolide antibiotic use.
- In studies reviewed by PubMed, LGG improved stool consistency and reduced frequency during antibiotic treatment.
3. Other Effective Strains
Additional strains also contribute to gut support during antibiotics:
- Bifidobacterium lactis Bb-12: Supports digestion and reduces AAD, according to ScienceDirect and PMC journals.
- Lactobacillus acidophilus CL1285: Demonstrates protective effects when combined with other strains.
- Multistrain formulations combining Lactobacillus and Bifidobacterium species offer enhanced protection, especially at higher doses.
Choosing the Right Dosage
Probiotic effectiveness is dose-dependent. Higher doses are often more protective, especially for people at greater risk of gastrointestinal side effects.
Recommended Dosages
| Strain | Effective Dose Range |
|---|---|
| L. rhamnosus GG | 10–20 billion CFU/day |
| S. boulardii I-745 | 5–10 billion CFU/day |
| Multistrain combinations | 20–50 billion CFU/day (combined) |
A comprehensive review in BMJ Open found that higher doses yielded better protection against AAD, particularly in individuals with a history of GI sensitivity or prior antibiotic complications.
If you’re already supplementing, make sure to check CFU counts on the label and ensure viability through the product’s shelf life.
Safety and Practical Tips
- Avoid simultaneous intake: Don’t wash down your antibiotic with a probiotic—always separate them.
- Choose clinically backed products: Look for probiotics that specify strains (e.g., LGG, I-745) and publish research on effectiveness.
- Check for other interactions: Just like with calcium supplements blocking antibiotic effectiveness or zinc supplements and quinolone antibiotic risks, always consult your healthcare provider when stacking supplements or prescriptions.
If you’re unsure, ask your doctor or pharmacist to recommend a strain and formulation tailored to your health profile and the type of antibiotic prescribed.
Conclusion
Taking probiotics with antibiotics is one of the most evidence-backed ways to protect your gut health during and after antibiotic treatment. Start probiotics on the same day as your antibiotics, space doses by 2–4 hours, and continue for at least a week after finishing.
The best strains for antibiotic support include Saccharomyces boulardii I-745, Lactobacillus rhamnosus GG, and Bifidobacterium lactis Bb-12. Aim for higher daily CFUs, especially if you’re prone to digestive discomfort.
Want to learn more about how supplements affect medication absorption? Explore our deep dive on calcium supplements and antibiotics.

