Certain supplements may reduce autoimmune symptoms – or worsen them – when combined with medications like methotrexate or biologics.
This article breaks down the science behind these interactions, helping you understand what to take, what to avoid, and when to consult your doctor.
If you’re navigating lupus, rheumatoid arthritis, or other autoimmune conditions, the right knowledge could make all the difference.
Summary / Quick Answer
Here’s a fast breakdown of supplement safety with autoimmune medications:
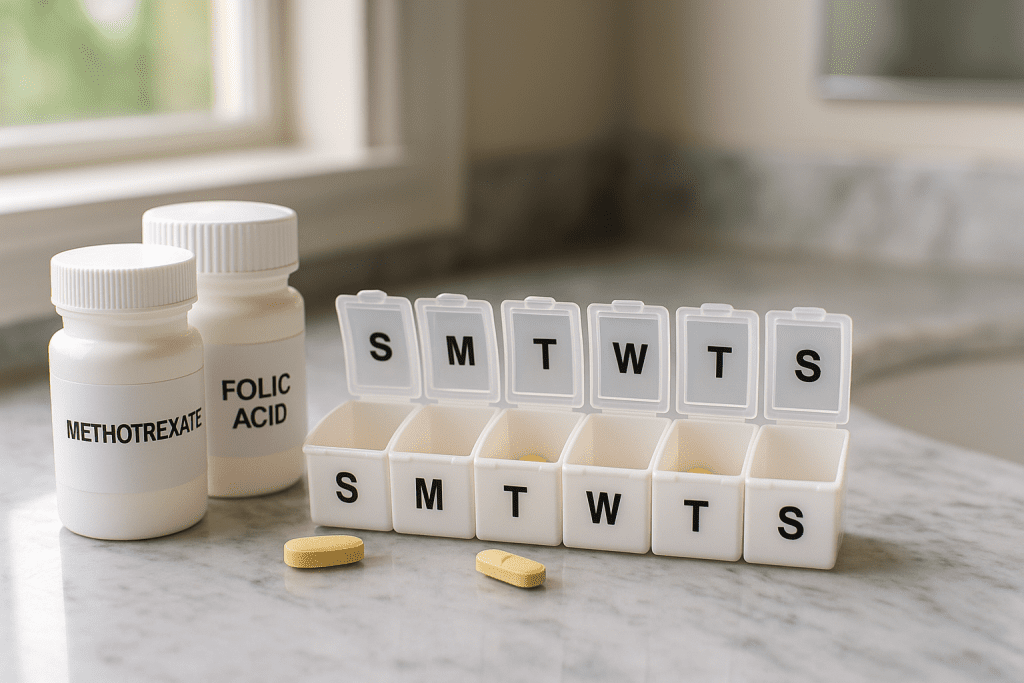
- Recommended with methotrexate: Folic acid, Vitamin D, Omega-3s, antioxidants (A, C, E)
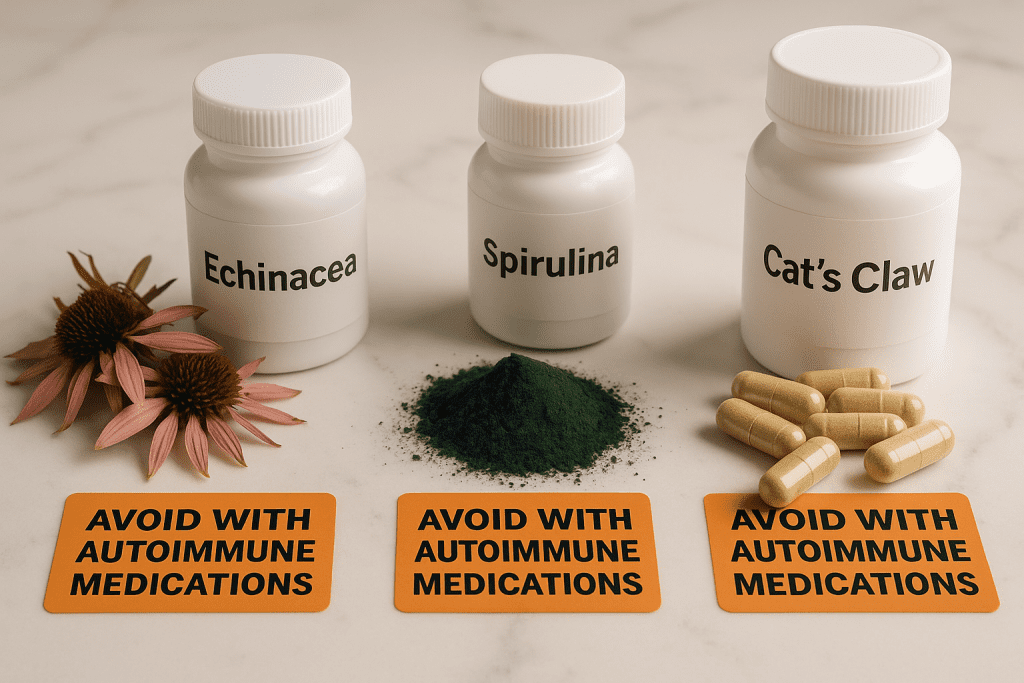
- Caution with herbs: Echinacea, St. John’s Wort, Cat’s Claw, Spirulina, Alfalfa
- Key rule: Avoid immunostimulatory herbs that may counteract immunosuppressants
- Timing tip: Take folic acid on a different day than methotrexate
- Medical oversight: Always consult a provider before starting any supplement
The autoimmune meds supplement conflict is real, but manageable with science-based choices.
How Autoimmune Drugs and Supplements Can Clash
Autoimmune diseases like lupus, rheumatoid arthritis (RA), and psoriatic arthritis often require medications that suppress overactive immune responses. Common treatments include:
- Methotrexate (MTX): A folate antagonist used in RA, psoriasis, and lupus
- Biologics: Drugs like adalimumab (Humira), etanercept (Enbrel), or infliximab (Remicade) that target specific immune pathways
- DMARDs: Disease-modifying antirheumatic drugs that reduce inflammation and slow progression
Many patients explore supplements to boost energy, immunity, or reduce joint pain – but combining them with prescription drugs can pose risks.
Why? Some supplements activate immune responses or alter how medications are absorbed or metabolized. This creates a biologics herbal interaction that may:
- Diminish drug efficacy
- Trigger disease flares
- Cause unexpected side effects
Think of it like tuning an orchestra: autoimmune drugs suppress immune activity, while certain herbs and vitamins turn the volume back up. The result? Discord and flare-ups.
Related: MyNetDiary vs. manual interaction tracking – a practical tool to log supplement-drug combos safely.
Let’s look at which supplements work in harmony – and which don’t.
Recommended Supplements for Autoimmune Patients

Folic Acid with Methotrexate
Methotrexate blocks folate metabolism to suppress immune cells, but this can lead to serious side effects like mouth sores, liver stress, hair thinning, and anemia. That’s where folic acid comes in.
Benefits of folic acid supplementation:
| Effect | Benefit |
|---|---|
| GI Tolerance | Reduces nausea, abdominal pain |
| Liver Health | Improves liver enzyme profiles |
| Treatment Continuity | Fewer dropouts from side effects |
| Anemia Prevention | Protects red blood cell formation |
The standard dose is 5 mg weekly, taken on a different day than methotrexate to avoid interfering with drug action.
According to NHS guidance, timing folic acid away from MTX reduces adverse events without reducing drug efficacy.
Vitamin D
Vitamin D plays a regulatory role in immune balance – and deficiency is common in autoimmune patients.
Research highlights:
- Low Vitamin D = higher autoimmune disease activity (meta-analysis)
- May reduce flares in lupus and early RA
- Binds to receptors on T and B cells, modulating inflammation
Optimal blood levels (30–50 ng/mL) are associated with improved treatment response. Check your labs and discuss dosing with your physician.
Omega-3 Fatty Acids
Omega-3s (from fish oil or algae) offer anti-inflammatory support and may boost DMARD or MTX effectiveness.
| Omega-3 Benefit | Supporting Evidence |
| Fewer tender joints | Clinical trials in RA patients |
| Improved lipids | Reduced triglycerides |
| Lower liver enzymes | Shown with MTX co-use |
| Possible remission boost | High-dose trials show doubled remission rate |
Aim for 2–5 grams/day EPA + DHA under medical supervision.
Read more: Omega-3 and methotrexate interaction studies.
Antioxidant Vitamins (A, C, E)
Oxidative stress is a key player in autoimmune flare-ups. Antioxidants may help.
A randomized trial found that combining vitamins A, C, and E with methotrexate significantly reduced joint swelling and improved Disease Activity Scores (DAS-28).
Note: Antioxidant use should be supervised. Megadosing can impair immunity or interact with other treatments.
Supplements to Avoid or Use with Caution
Immunostimulatory Herbs
Herbs like Echinacea or Spirulina are marketed for “immune boosting,” but for autoimmune patients, that’s a red flag.
| Herb | Risk |
| Echinacea | May reduce MTX efficacy and trigger flares |
| Spirulina | Stimulates cytokine production, worsens inflammation |
| Chlorella, Alfalfa | Linked to lupus flares and immune activation |
A case report linked Echinacea to pemphigus flare in a stable patient. These botanicals can counteract the intended suppression of your medications.
St. John’s Wort
This herb impacts liver enzymes (notably CYP3A4), altering drug metabolism.
Animal studies show that combining St. John’s Wort with methotrexate increased drug toxicity and mortality.
According to PubMed research, it raised methotrexate plasma levels by 163%.
It can also interfere with biologics or corticosteroids by speeding their breakdown or increasing side effects.
Cat’s Claw
While Cat’s Claw shows anti-inflammatory effects, it stimulates immune cells and may:
- Counteract immunosuppressants
- Increase bleeding risk (especially with blood thinners)
- Cause interactions in transplant patients
Source: Mount Sinai notes caution for all immunocompromised individuals.
Hidden Folic Acid in Multivitamins
Patients already prescribed folic acid should avoid over-supplementing with multivitamins or fortified foods.
Excess folate could interfere with methotrexate’s intended action or mask anemia from B12 deficiency.
Checklist:
- Read labels on all vitamin products
- Check with your doctor before combining sources
- Track doses using manual interaction tracking tools
Smart Supplement Practices for Autoimmune Care
Timing Is Everything
For methotrexate users:
- Take folic acid at least 24 hours apart from your MTX dose
- Many doctors recommend taking it 48 hours before or after to reduce nausea
- Stick to weekly dosing unless advised otherwise
For other supplements:
- Space dosing to avoid overload on the liver or kidneys
- Track how supplements affect labs, energy, and symptoms
Medical Supervision Is Non-Negotiable
Always:
- Inform every provider (dentist, pharmacist, nutritionist) about your autoimmune meds
- Bring a treatment card or list to all appointments
- Ask before starting anything new – including herbs or over-the-counter blends
Why? Even natural substances can carry risk. Interactions aren’t always obvious, especially with new biologics or combo therapies.
Conclusion
Autoimmune conditions often require a delicate balance between suppressing the immune system and supporting overall health. When used properly, supplements like folic acid, vitamin D, omega-3s, and antioxidants can improve medication tolerance and disease control. However, herbal remedies like Echinacea, Cat’s Claw, and St. John’s Wort may pose hidden risks.
Your safest path? Stay informed, monitor your supplement-drug interactions, and check every addition with a provider. To track your intake efficiently, explore MyNetDiary vs. manual interaction tracking – a helpful way to avoid mistakes before they happen.

