If you’ve ever taken a zinc supplement alongside antibiotics and felt queasy, you’re not alone. This article breaks down the science behind that stomach-churning combo, including why it happens and how to avoid it.
We’ll explore how zinc and certain antibiotics interact to trigger nausea, what adjustments in timing or diet can help, and how to get the benefits of both with fewer side effects. Whether you’re on tetracyclines or just prone to stomach issues, we’ve got expert-backed strategies to help.
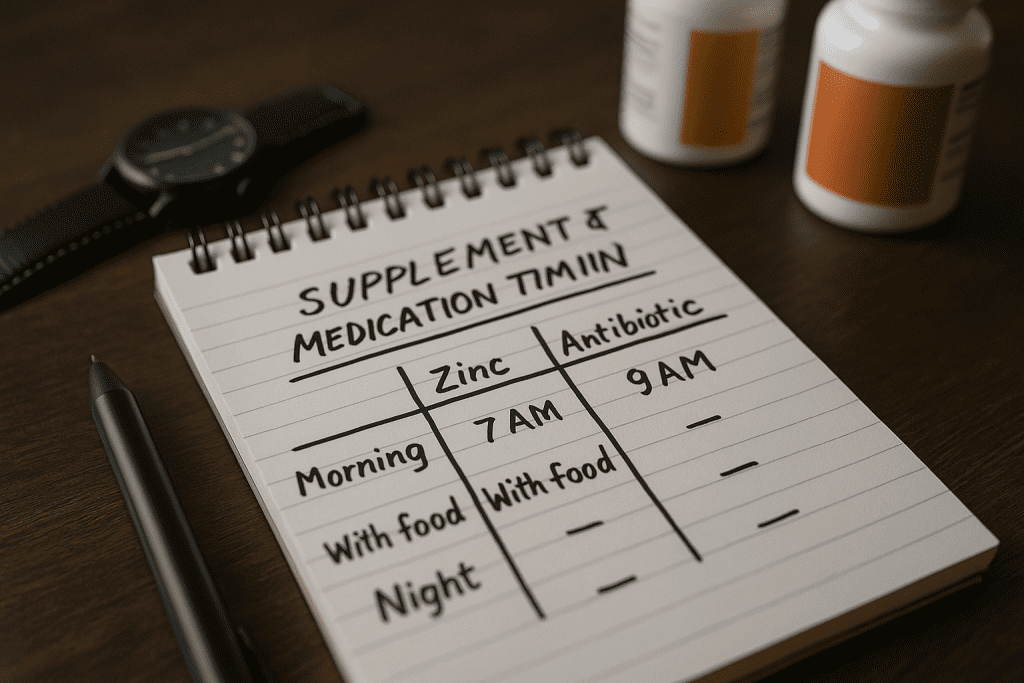
Quick Summary: Why Zinc and Antibiotics Cause Stomach Issues
| Problem | Cause | How to Fix It |
|---|---|---|
| Zinc antibiotic nausea | Chelation between zinc and antibiotics disrupts absorption | Take antibiotics 2 hours before or 6 hours after zinc |
| GI upset supplement combo | Both zinc and antibiotics irritate the stomach individually | Take with food when possible; stay hydrated |
| Zinc pill stomach issues | Zinc irritates gastric lining, especially on an empty stomach | Choose gentler zinc forms like zinc gluconate; lower the dose |
| Gut health disruption | Antibiotics kill good bacteria, worsening stomach symptoms | Add probiotics; see probiotic and antibiotic timing guidelines |
Why Zinc and Antibiotics Often Don’t Mix

Chelation: A Hidden Absorption Problem
Zinc and antibiotics—particularly tetracyclines like tetracycline and doxycycline—can form a chemical bond in your gut known as a chelate. This zinc-antibiotic chelate isn’t well absorbed, meaning the antibiotic might not work as effectively. According to research published in PubMed, zinc reduced tetracycline absorption by about 30%, which could compromise your infection treatment.
Doxycycline, a newer tetracycline, seems less affected by zinc in some studies, but the interaction still poses a risk for GI upset. Other antibiotics, like erythromycin, aren’t affected by chelation but still irritate the stomach.
Dual Digestive Irritants
Even without chelation, zinc and antibiotics can independently wreak havoc on your stomach:
- Zinc can cause nausea, vomiting, cramps, and diarrhea—especially if taken without food. A clinical trial showed zinc-induced vomiting within just 10 minutes in some patients.
- Antibiotics like tetracyclines and macrolides (e.g., erythromycin) disrupt gut flora, irritate the stomach lining, and can cause acid reflux or nausea.
Together, this combo can overwhelm your gut and lead to persistent discomfort.
Timing and Food: Your Best Defenses
Adjust Your Schedule to Reduce Risk
The simplest and most effective fix? Don’t take zinc and antibiotics at the same time. According to dosing guides from Drugs.com, it’s best to:
- Take antibiotics at least 2 hours before or 6 hours after any zinc supplements.
This window reduces the chance of chelation and allows both substances to absorb effectively.
If you’re taking an antibiotic that already causes GI upset—even without zinc—this timing trick can also prevent compounded irritation.
Eat Something First (When Allowed)
Food is a natural buffer. It helps minimize direct irritation from both antibiotics and zinc. While some antibiotics require an empty stomach for best absorption, others can be taken with meals:
- Zinc: Always take with food, unless instructed otherwise. This reduces the likelihood and intensity of nausea (CORR HEAL).
- Antibiotics: Check your prescription. Many allow or even recommend taking with food to ease stomach upset.
For those that don’t, wait about 30 minutes post-dose before eating.
Gut-Friendly Foods and Supplements
Support your digestion during antibiotic treatment with these additions:
- Probiotics: Protect your gut flora and reduce antibiotic-related diarrhea. See our probiotics and antibiotic timing guidelines.
- Fiber: Foods like oats and bananas can help settle your stomach.
- Hydration: Drink a full glass of water with every dose.
Choosing Better Formulations and Doses
Not all zinc supplements hit your stomach the same way. Formulation matters:
| Zinc Type | GI Tolerance Level | Notes |
| Zinc sulfate | Low | Most likely to cause nausea and cramping |
| Zinc gluconate | Moderate | Often better tolerated, easier on stomach |
| Zinc picolinate | High | Good absorption, gentler than zinc sulfate |
In general, lower doses are safer for sensitive stomachs. If you’re not zinc-deficient, you may not need high-dose supplements at all.
Extended-release or buffered formulations of both zinc and antibiotics may also reduce peak irritation.

Special Considerations for Sensitive Groups
Some people are simply more prone to zinc antibiotic nausea. Factors that increase susceptibility include:
- Gender: Women may experience more zinc-related nausea than men (Consensus).
- Body Size: Smaller individuals may feel stronger side effects from standard doses.
- Existing GI Conditions: Ulcers, IBS, or acid reflux can heighten irritation.
- Elderly Patients: Often have reduced stomach acid, altering absorption.
If you fall into one of these groups, talk to your doctor before starting any zinc-containing supplement during antibiotic therapy.
When to Call Your Doctor
Mild nausea is common. But if symptoms are severe or last more than a few days, reach out to your healthcare provider. In some cases, adjusting your dose, switching formulations, or changing your antibiotic may be necessary.
For example, if you’re taking calcium along with zinc, you might also want to read about how calcium supplements block antibiotic effectiveness. Understanding all your supplement-drug interactions can prevent unwanted side effects.
Final Thoughts
Zinc and antibiotics each play a role in health, but together they can upset your stomach more than you’d expect. By spacing them out, taking them with food when possible, and choosing better-tolerated formulations, you can significantly reduce nausea and discomfort.
If you’re navigating multiple supplements and medications, tools like our probiotics and antibiotic timing guide make it easier to stay on track. And always consult a healthcare professional before starting new combinations.

